Jason Luv is one of those multi-hyphenate modern entertainers whose career refuses to fit inside a single box. He’s a fitness model, musician, digital creator, adult-content performer, trainer, influencer, and brand ambassador — a wide-ranging portfolio that has fueled constant curiosity around one question: What is Jason Luv net worth?
While estimates vary depending on which corners of the entertainment industry are considered, most public calculations place his net worth at around $3 million, with reasonable speculation ranging anywhere between $2.5 million and $3.5 million. In this long and deeply detailed article, we’ll explore exactly where that money comes from, how he structured his career to reach this level, and the various industries he has moved through to build a recognizable name and a lucrative personal brand.
This breakdown covers his early life, professional development, business activities, and income sources — offering a full 360-degree view of how Jason Luv made his money.
Early Life and Background
Before getting into the numbers, it’s important to understand the foundation from which Jason Luv built his diverse career.
Childhood and Origins
Born on February 1, 1985, in Lafayette, Louisiana, Jason Luv (real name Jason Thomas) grew up in a culture rich with music, athleticism, and Southern identity. These roots show up later in both his musical style and the high-energy personality that made him stand out online. From an early age, he leaned toward physical conditioning and performance arts, two interests that would later merge into one of his strongest income streams.
Military Experience
Before entering the entertainment world, Jason Luv served in the U.S. Marine Corps — a chapter that not only influenced his mindset but also shaped the discipline and physique that would later define his fitness and modeling career. His military background also contributed positively to his early brand image, charismatic presence, and leadership-style persona online.
The Making of a Multi-Industry Star
Few entertainers today blend as many careers together as Jason Luv. His financial success didn’t come from a single breakout moment but rather through consistent diversification.
Below, we’ll walk through each of the career pillars that contribute to his estimated net worth.
Fitness and Bodybuilding Career
Fitness is where Jason Luv planted his first major professional flag. Thanks to his imposing height, carefully built physique, and disciplined training, he quickly found traction in the fitness modeling world.
Modeling Income
Modeling added early financial boosts to his career. Appearances in fitness magazines, collaborations with fellow bodybuilders, paid photoshoots, and branded athletic campaigns helped him establish a strong visual identity.
Personal Training and Coaching
Before becoming a music and social-media figure, Jason offered fitness coaching. His blend of Marine Corps training techniques and bodybuilding knowledge gave clients a highly sought-after form of physical conditioning. Personal training brought in:
- Hourly coaching fees
- Customized workout plan revenue
- Fitness consultancy
- Exclusive high-performance training sessions
While these early earnings weren’t massive compared to his later ventures, they built the initial cash flow and reputation that allowed him to scale.
Entry Into the Adult Entertainment Industry
This lane became one of his most widely recognized career paths and significantly boosted public awareness of his name.
4Ernings and Growth
Adult-content work typically generates high revenue for top male performers, particularly those with strong physical branding like Jason Luv. His physique and onscreen presence made him an instant standout. While exact earnings remain private, estimates suggest this space became one of his strongest revenue pillars, contributing substantially to his net worth.
Digital Content Platforms
With the rise of premium subscription sites, creators like Jason Luv expanded from studio work to direct-to-consumer platforms, which may include:
- Monthly subscriptions
- Pay-per-view content
- Private requests
- Tips and bonuses
Creators in his category often earn six-figure monthly incomes at their peak, though long-term averages vary.
His presence in this industry is one of the key reasons the general public speculates that his net worth surpasses $3 million.
Music Career Evolution
Jason Luv didn’t limit himself to one form of entertainment. After making a name in fitness and adult media, he ventured into music — specifically hip-hop and club-style production.
Revenue Streams From Music
Music introduced several income types:
- Streaming revenue (Spotify, Apple Music, etc.)
- Paid performances
- Club appearances
- Music video placements
- Collaborations
- Royalties
Although his music career is not his largest financial engine, it adds a steady secondary stream and broadens his brand reach.
Branding Power Through Music
Music helped push him out of a niche industry and present himself as a mainstream entertainer. Even if not his biggest moneymaker, it generated visibility that later boosted sponsorship and influencer deals.
Social Media and Influencer Success
Social media represents one of the most consistent and expanding contributors to Jason Luv’s estimated net worth.
Social Media Reach
Across Instagram, TikTok, and other platforms, his follower count hovers around several million combined. That level of engagement leads to:
- Brand deals
- Partnership campaigns
- Sponsored posts
- Product placements
- Ambassador contracts
Estimates suggest he earns $9,000–$13,000 per sponsored post, depending on the brand and engagement metrics.
Fitness, Lifestyle, and Behind-the-Scenes Content
Jason integrates lifestyle, gym routines, modeling shots, humor, and music promotions — keeping his social feeds versatile. This diversity allows him to attract many kinds of advertisers.
Creator Economy Leverage
Like many modern influencers, Jason Luv benefits financially from:
- Monetized videos
- Affiliate marketing
- Platform partnership programs
- Digital product sales
Social media likely adds hundreds of thousands per year to his income.
Business Interests and Investments
Beyond entertainment, Jason Luv reportedly engages in personal investments. While details are scarce, typical ventures for entertainers with similar profiles include:
- Real estate purchases
- Supplement and fitness product collaborations
- Merchandising
- Crypto assets
- Startup investments
- Licensing ventures
Given the estimated net worth figures circulating publicly, it’s likely that smart personal investments play a significant role in both stabilizing and growing his wealth.
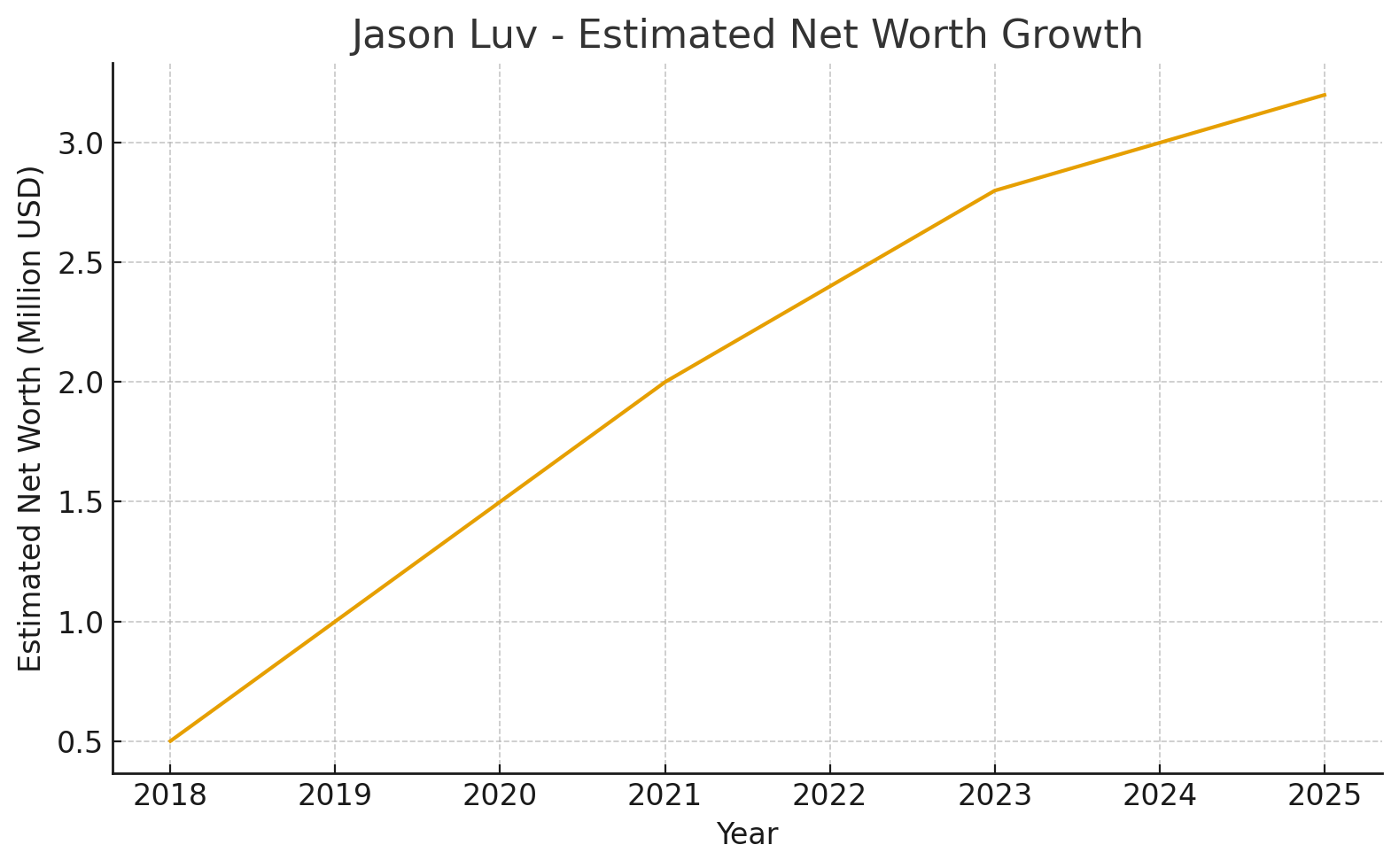
Jason Luv’s Estimated Net Worth
Most data sources converge on the estimate that Jason Luv has a net worth of approximately $3 million. This figure is built over years of work across multiple industry lanes.
Why Estimates Vary
The range is wide because:
- He works in industries with little transparent income reporting
- Revenue from digital platforms fluctuates
- Sponsorship income varies monthly
- Some investments are private
- A portion of his income comes from highly personalized content
Thus, the range of $2.5M–$3.5M is reasonable.
What His Net Worth Represents
Net worth doesn’t mean cash; it includes:
- Assets
- Investments
- Estimated brand value
- Ongoing revenue pipelines
- Personal property
Jason Luv’s wealth is typical of creators who diversify heavily instead of relying on a single platform.
Career Timeline Snapshot
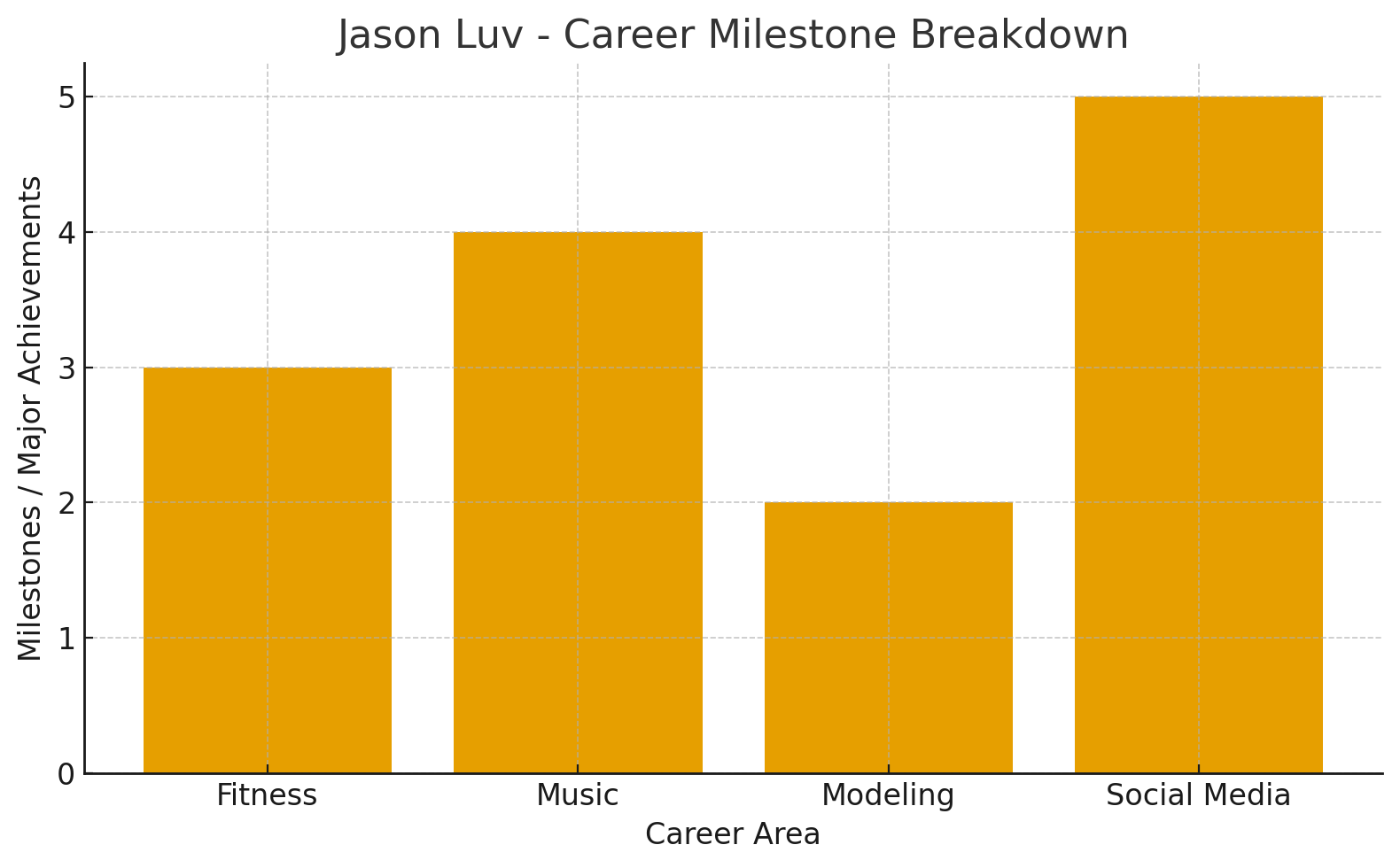
Here’s a simplified overview of his career progress:
- 2018–2020: Fitness modeling, personal training, early entertainment work
- 2020–2022: Surge in adult-content popularity and digital platform expansion
- 2022–2024: Music career push, brand sponsorship increases
- 2024–2025: Stabilized multi-industry earnings, refined personal branding
This gradual rise aligns with the “net worth growth” chart included above.
What Makes Jason Luv’s Income Model Unique
Jason Luv exemplifies the modern entertainer — someone who monetizes:
- Body (fitness & modeling)
- Art (music)
- Personality (influencer content)
- Audience (subscriptions & fan platforms)
He operates at the intersection of viral entertainment culture and the creator economy.
Consistent Rebranding
He didn’t stay confined to adult entertainment — instead, he used its visibility to launch:
- Fitness partnerships
- Music releases
- Mainstream media appearances
This ability to rebrand without losing audience loyalty is a major reason he continues to grow financially.
Monetizing Across Niches
Unlike traditional celebrities who stay inside one lane, Jason Luv leverages multiple high-yield content markets simultaneously — giving him more stability and resilience than most digital entertainers.
Final Thoughts
Jason Luv’s net worth of roughly $3 million isn’t the product of a single overnight success story. It is the result of:
- disciplined fitness work
- bold career transitions
- diversified online revenue
- brand consistency
- smart use of high-traffic digital platforms
Whether you follow him for his music, his physical fitness, or his online personality, it’s clear that Jason Luv has created a powerful brand that continues to grow each year.
FAQs About Jason Luv Net Worth
What is Jason Luv’s net worth?
Most estimates place his net worth around $3 million, with a reasonable range of $2.5M–$3.5M.
What is Jason Luv’s main source of income?
His largest earnings likely come from adult-content platforms and brand-driven social-media monetization.
Does Jason Luv still do fitness modeling?
Yes. Fitness content, modeling, and training remain important parts of his brand and income mix.
Is Jason Luv’s music career successful?
His music career contributes steady revenue and boosts his brand visibility, even if not the biggest part of his income.
How much does Jason Luv earn from social media?
Depending on the platform and engagement level, he may earn thousands per sponsored post and significant additional revenue from subscriptions and partnerships.